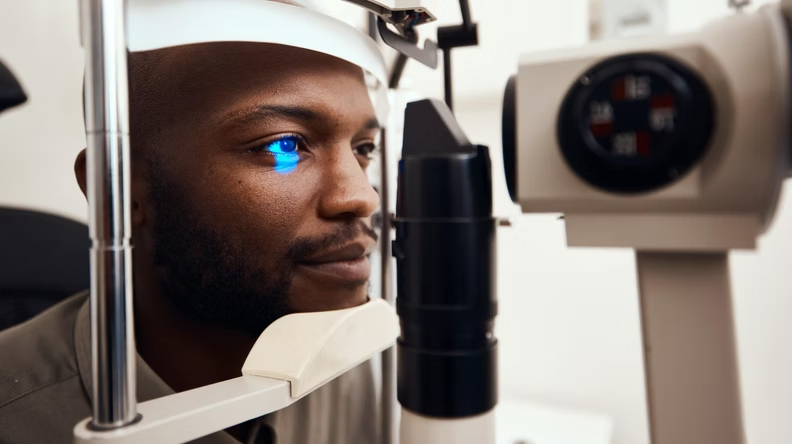
It is important that eye tests are performed regularly for early detection of symptoms of glaucoma. If early symptoms are discovered within routine eye tests, patients can be referred to an ophthalmologist to give confirmation on their diagnosis. An ophthalmologist can then provide information for case-by-case specifics, along with treatment advice.
Diagnosing glaucoma is not always an easy task as there are a magnitude of factors that can go into having this eye condition. To combat this, there are a range of different ways it can be identified and tested for:
Eye Pressure Check (Tonometry)
One of the largest risks of glaucoma is an increase in eye pressure. This is commonly the biggest sign of glaucoma and is often conducted through Tonometry, the most popular method being ‘The Goldmann applanation tonometry test. During which, eyes drops are administered and then a flat-tipped probe is lightly pressed against the surface of the eye into the cornea. The cornea will then push back onto the tonometer and the pressure that is produced is measured, giving a number for the patient which can be compared each year to monitor potential glaucoma.

“In England, about 480,000 people have chronic open-angle glaucoma.”
Visual Field Test (Perimetry)
This test is performed one eye at a time whilst the other is covered, so not to produce any errors within the results. The test involves a light that repeatedly focuses on different areas of the patient’s peripheral vision. It will then show the extent of their visual field that each eye can see. It can detect a lack of function within both central and peripheral vision, thus caused potentially by glaucoma or other neurological conditions.
“Approximately 10% of UK blindness registrations are ascribed to glaucoma. It is estimated that in the UK about 2% of people older than 40 have chronic open angle glaucoma, and this rises to almost 10% in people older than 75.”
Cornea Thickness Test (Pachymetry)
If a patient is getting artificially low eye pressure readings, then the thickness of their cornea may be influencing these results. Pachymetry is performed by firstly administering eye drops and then gently placing a pachymeter (a small probe) onto the cornea, to correctly measure how thick it is. This is measured on both eyes and if a thick cornea is detected, then this information can help to understand eye readings on other tests, to ensure an accurate evaluation is achieved.
Angle Test (Gonioscopy)
An angle test inspects the space between the iris and the cornea. The eyes will initially be numbed with drops and then a gonioscopy lens is placed onto the eye. This then measures whether the space between the iris and cornea is narrow or broad. If the result is narrow, then this could be a symptom of acute glaucoma, whilst a wide result could be a symptom of chronic glaucoma.
We regularly see and treat glaucoma patients and in the past 3 months have treated over 2,000 patients. For information on our ophthalmology services, please visit: www.healthharmonie.com/ophthalmology
We also provide outsourcing to hospitals for glaucoma wait list support. We offer these through the NHS increasing capacity framework. More information on the subject: www.healthharmonie.com/nhs-partnership